Introduction to Clinical Trials
The journey to bring innovative medical treatments from concept to clinic is a sophisticated and closely monitored road that is vitally important for advancing medicine and patient care. At the helm of this process lies the clinical trial, a meticulously designed research study to answer specific health questions. What is a clinical trial? These trials are systematic procedures that comply with stringent regulatory guidelines to guarantee the safety and effectiveness of a possible new drug or treatment. As pillars of evidence-based medicine, these trials serve not only to test new medical interventions but also to continually refine and optimize standard care practices. Ethical considerations underscore this entire process, as the rights and welfare of human participants are of paramount concern. From Phase 1 trials, which focus on safety and dosing, to the larger-scale and more complex Phase 3 trials, clinical studies provide the data and insights necessary to make informed decisions about the future of healthcare interventions. It is not an understatement to say that clinical trials are the essential conduits of modern medicine.
Pre-Clinical Research
Every clinical trial originates from a thorough groundwork phase known as pre-clinical research. This precursor to human trials encompasses various laboratory tests and experiments on animal subjects. These are crucial for establishing a baseline understanding of how a new compound or medical device behaves biologically. These initial stages allow scientists to glean essential information about a treatment’s potential effects, toxicity levels, and pharmacokinetics, which is how a substance enters, moves through, and exits the body. This phase is no mere formality; it is a highly controlled and critiqued series of tests designed with the utmost attention to ethical animal use and relevance to human health. Only when a compound successfully demonstrates a favorable balance between potential efficacy and safety in this pre-clinical stage is it considered for trials within the human populace, marking the transition from laboratory to clinic?
Phase 1: Safety and Dosage
As a drug or treatment enters the clinical trial phase, it embarks on a preliminary yet critical exploratory study encompassing a small cohort of participants, often healthy volunteers. Phase 1 trials aim to identify the ideal dosage range that minimizes risks and maximizes potential therapeutic effects, as well as to assess the safety profile of the intervention. It sets the foundational parameters upon which all subsequent trial phases will build.
Researchers meticulously evaluate every outcome at this juncture, searching for any hint of adverse reactions or unexpected challenges. These initial human subjects are monitored with intense precision, as their experiences will chart the course for every step that follows in the drug development pipeline.
Phase 2: Efficacy and Side Effects
Upon securing a favorable safety report from Phase 1, a therapy moves into the second phase, where the waters of efficacy are tested. Phase 2 trials are pivotal in assessing whether the drug or treatment is effective for its intended purpose and further investigating side effects. A larger group of participants is enrolled and monitored, establishing the first evidence base for clinical effectiveness. This stage is crucial for fine-tuning the drug’s application, refining dosing protocols, and gathering data on how different populations may respond to the treatment. It is within Phase 2 that the promise of a new therapy starts to crystallize as researchers untangle the complexities of its impact on human health.
Phase 3: Confirmation and Comparison
The final hurdle before therapy can seek regulatory approval is Phase 3, a comprehensive and rigorous trial phase that aims to solidify and confirm the findings from earlier phases. Regarding scale, Phase 3 is significantly larger than its precursors, involving a cross-section of the population across multiple locations. Here, the drug is administered to thousands of patients, providing substantial evidence about its effectiveness, benefits, and side effects compared to standard treatments. The drug is tested under real-world conditions in these expansive studies, allowing researchers to verify its value across diverse groups and situations, echoing the variability in broader patient communities. These robust data help shape tomorrow’s healthcare decisions and are the basis upon which approval for public use is granted.
Phase 4: Post-Market Surveillance
Even after a drug has been approved for the market, it remains under vigilant scrutiny. Phase 4, or post-market surveillance, plays an essential role in the lifecycle of a medical treatment. This phase ensures ongoing evaluation of the drug’s performance when utilized within the general population—a larger and more varied audience than any clinical trial can replicate. It helps to capture any long-term effects or rare adverse events that may not have been evident in controlled trial settings. Safety protocols in clinical trials are meticulously followed during this stage, ensuring that the well-being of patients continues to be a top priority and that any risks are identified and managed proactively. The information gathered from this open-ended phase is invaluable, often resulting in updates to treatment guidelines, labeling changes, or, in some cases, revocation of the treatment’s approval. As such, Phase 4 trials serve as a vital safety net for the medical community.
Participant Selection Process
Who gets to participate in a clinical trial, and how are they chosen? These are critical questions at the core of the participant selection process. Each potential volunteer must meet specific inclusion criteria relevant to the trial, such as age, gender, health status, and sometimes even genetic markers. These criteria are not just about refining the study outcomes but also about ensuring safety and reducing the risk to the individuals involved. The informed consent process, whereby participants are fully informed about participation—including potential risks, benefits, and alternatives—is the ethical cornerstone of participant selection. It ensures that individuals make educated decisions about their involvement, upholding the pillars of autonomy and respect within clinical research.
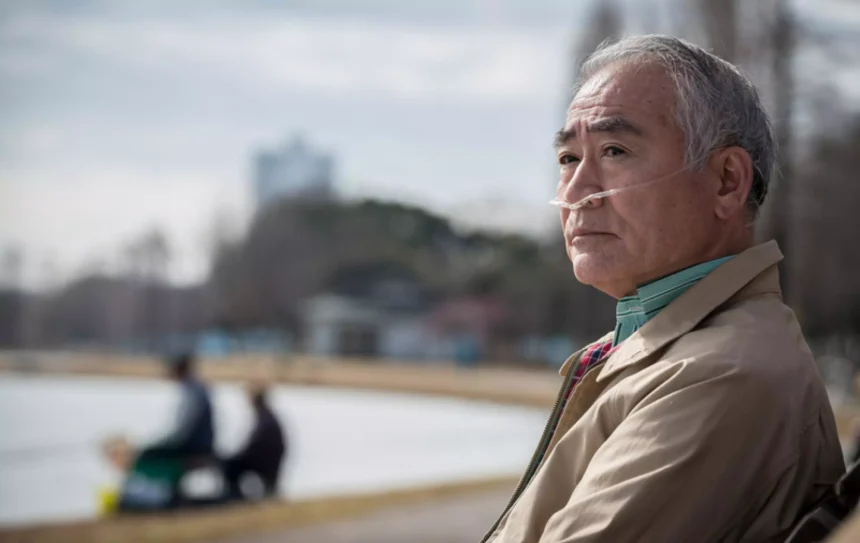
Ensuring Participant Safety
Paramount in the hierarchy of considerations during a clinical trial is the safety and well-being of participants. A network of ethical guidelines, safety protocols, and oversight bodies converge to create a framework aimed at minimizing risk and ensuring that the rights of participants are upheld. At every step of the way, from preliminary screenings to post-trial follow-ups, vigilant measures are in place to protect against potential harm and ensure that adverse events are properly managed and systematically reported. In the event of any unexpected reactions or complications, swift action is taken to reassess the situation and, if necessary, adapt the study protocols or provide immediate medical intervention to the participant. Continuous monitoring, regular health assessments, and open communication support the safety of those involved in clinical trials.
The Role of Regulatory Bodies
Regulatory standards for the highly structured field of clinical research are established by the US Food and Drug Administration (FDA) and its international counterparts. These regulatory entities provide:
- A critical oversight role.
- Setting forth regulations.
- Reviewing collected data for accuracy and reliability.
- Ensuring that each clinical trial phase is conducted according to stringent ethical principles and scientific rigor.
Adherence to global guidelines, like Good Clinical Practice (GCP), is imperative to guarantee a consistent lineage of clinical trial management and safeguarding of participants. The public’s confidence in the medical research establishment is maintained, and regulatory bodies play the vital role of protecting clinical integrity by ensuring that the goals of clinical trials—to ascertain the safety and efficacy of novel treatments—are not jeopardized.
The Future of Clinical Trials
The field of clinical trials is not static; it is ever-changing, with continuous enhancements reshaping methodologies and improving efficiency. Technological advances, such as electronic data capture, mobile health applications, and remote monitoring, are revolutionizing the infrastructure of clinical studies. These innovations are streamlining processes, making trials more accessible, and providing richer, high-quality data at a pace never seen before. As the scientific community and stakeholders embrace these shifts, the evolving landscape of clinical trial methodologies promises to accelerate the delivery of treatments from bench to bedside, propelling medicine into a future where therapies are more personalized, outcomes are more successful, and patient care is more effective than ever.
The digital transformation of clinical trials is not merely a matter of convenience; it can democratize trial access, increase participant diversity, and foster a more holistic and responsive approach to therapeutic development. This momentum reinforces the inherent optimism of the clinical trial process: that through dedication, innovation, and unyielding commitment to safety and ethics, the horizon of medical possibilities will continue to expand, improving lives around the globe.